
The neurology market is undergoing an unprecedented transformation, driven by both technological advancements and changing patient expectations, as revealed by consumer behavior studies. Neuromarketing isn’t just a buzzword anymore; it represents a fusion of market research and consumer neuroscience that has redefined how brands approach customer engagement. The rising interest in tools like eye-tracking, EEG […]

The neurology market is undergoing an unprecedented transformation, driven by both technological advancements and changing patient expectations, as revealed by consumer behavior studies.
Neuromarketing isn’t just a buzzword anymore; it represents a fusion of market research and consumer neuroscience that has redefined how brands approach customer engagement.
The rising interest in tools like eye-tracking, EEG facial coding, and fMRI highlights the industry’s focus on decoding emotional responses and enhancing decision-making processes.
With the global neurology market projected to more than double from $3.88 billion in 2025 to $7.57 billion by 2034, practices face both significant opportunities and competitive pressures.
It isn’t just about adopting new neuromarketing techniques; it’s about understanding that neurological patients face unique challenges that traditional healthcare delivery often fails to address.
Unlike other medical conditions, where patients can see and monitor their progress, neurological conditions affect the brain, an organ that patients cannot observe or easily understand. This creates unique challenges that require a shift from traditional market research to more innovative approaches, such as focus groups enhanced by neuroscientific insights.
The following trends represent practical strategies that successful neurology practices are using to meet patients where they are, both technologically and emotionally, while building sustainable competitive advantages in an increasingly crowded marketplace.
The global market size of neurology was estimated at USD 3.60 billion in 2024 and is predicted to increase to USD 3.88 billion in 2025, with projections to reach approximately USD 7.57 billion by 2034, expanding at a Compound Annual Growth Rate (CAGR) of 7.72% from 2025 to 2034.
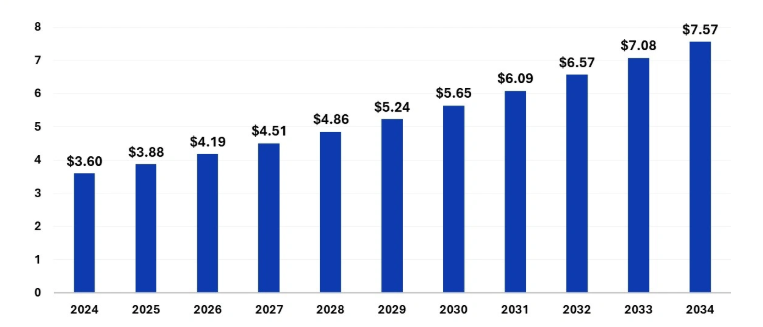
The U.S. neurology therapeutics market size was evaluated at USD 1.04 billion in 2024 and is projected to be worth around USD 2.31 billion by 2034. The market is growing at a CAGR of 8.31% from 2025 to 2034.
North America contributed more than 42% of the global neurology market share in 2024, making it the largest regional sector in the market segmentation.
Over 7 million people in the U.S. were living with Alzheimer’s disease in 2024, expected to increase to nearly 13 million by 2050, and approximately 1 million people in the U.S. were living with Parkinson’s disease in June 2024, projected to grow to 1.2 million by 2030. The increasing prevalence of neurological disorders is a key driver for growth in neurology market in 2025.
According to neuromarketing research, the global digital health in neurology market is valued at USD 39.6 billion in 2024 and is projected to reach USD 281.0 billion by 2034, growing at a 21.8% CAGR during the forecast period from 2025 to 2034.
Over 60% of users now access healthcare information through mobile devices.
Over 40% of patients now schedule medical appointments online.
71% of people research healthcare providers through digital channels, which is the most significant contributing factor to their decision-making.
Telehealth is rapidly gaining traction in neurology for accessibility, with 98% of neurologists offering virtual consultations and 36% of neurological visits now taking place online.
Here are the key trends in neurology care marketing:
Your patients are juggling work, family, and a neurological condition that already disrupts their lives enough.
The last thing they want is to take another afternoon off, sit in traffic, and spend two hours at your office for a 15-minute medication check.
Your migraine patients might be having breakthrough headaches but putting off scheduling because they can’t afford another day away from work. Your epilepsy patients might question whether their medication side effects warrant a visit, so they are suffering in silence or turning to Google for answers.
To provide them with a human solution, start conversations with your current patients about telemedicine. Ask them directly: “What would make managing your condition easier?” You will hear things like, “I wish I could just check in with you when my symptoms change,” or “It’s so hard to get here during business hours.”
When rolling out telemedicine, don’t lead with the technology; lead with understanding. Your marketing should sound like this: “We know that living with chronic migraines means unpredictable days. That’s why we are bringing care to you, whether you are having a good day or struggling through a bad one.”
Find patients who have genuinely benefited and let them tell their stories in their own words. Not polished testimonials, but honest conversations like “I can actually talk to Dr. Smith when I am having symptoms instead of waiting weeks for an appointment when I feel fine again.”
Picture this: It’s 11 PM, and someone’s experiencing numbness in their arm for the first time, prompting an urgent need for understanding their brain activity.
They are scared, they are Googling, and they are probably convincing themselves they are having a stroke. Where do you want that person to land?
People are using symptom checkers because they are worried, confused, or can’t wait until morning for answers. Your AI tool needs to speak to that fear, not just collect data.
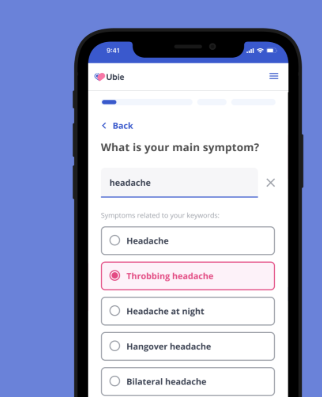
Try to make it human. Instead of clinical questionnaires, start with empathy: “Neurological symptoms can be scary. Let’s figure out what’s going on together.” Guide them through questions the way you would in person, explaining why you are asking, what you are looking for, and what different answers might mean.
When someone reports concerning symptoms, don’t just say, “Seek immediate care.” Explain why: “These symptoms can sometimes indicate something that needs quick attention. Here’s what we would want to rule out…” This teaches while it guides.
The real win is when patients arrive for their appointment, they are not starting from zero.
They have already experienced your clinical thinking, your communication style, and your genuine concern for their wellbeing. You are not just another doctor; you are the neurologist who was there when they were scared and needed answers, influencing their subconscious trust in your care.
Your AI tool becomes a bridge, not a barrier. It says things like, “I understand you are worried about these headaches. Here are some questions that will help us understand what’s happening, and here’s why each one matters.” It makes patients feel heard before they have even spoken to a human.
Here’s the thing about neurological conditions: they are happening inside the one organ that patients can’t see or touch.
Someone with diabetes can monitor their blood sugar and see immediate feedback. But when you have epilepsy, migraines, or Parkinson’s, your brain feels like this mysterious black box that’s betraying you.
The real problem is that your patients leave appointments with more questions than answers. They nod along when you explain neurotransmitters and neural pathways, but they are thinking, “What does this mean for me?” They go home and immediately Google everything, often landing on forums that scare them more than help them.
Stop talking about the brain and start helping people connect with their brain. When hosting a workshop on migraines, don’t just lecture about triggers; have participants track their own patterns in real time. Give them the same tools you use to think about their condition.
Picture a Parkinson’s workshop where patients aren’t sitting passively in chairs. They are doing the same coordination exercises you use in assessments, but now they understand why. When someone struggles with a task, they are not just failing; they are learning: “Oh, this is what my doctor sees when she asks me to do this.”
The magic moment is when a patient says, “I finally understand what’s happening in my head.” Not just the medical explanation, but the lived experience that makes sense.
When someone with memory concerns engages in cognitive exercises alongside others facing similar challenges, they realize they are not “losing their mind” but are dealing with a specific and manageable issue.
To make it practical, you can opt for partner exercises with real understanding. When participants do memory games, explain: “This is working the same part of your brain that we are supporting with your medication.” When they practice balance exercises, connect it by saying, “These movements help strengthen the neural pathways we talked about in your appointment.”
Also See: Top 20 Healthcare Marketing Agencies to Boost Your Brand in 2025
Let’s cut through the buzzwords and talk about what’s really keeping your patients up at night. It’s not whether you are using the latest technology; it’s whether your patients’ most personal medical information is safe from hackers, insurance discrimination, or ending up in the wrong hands.
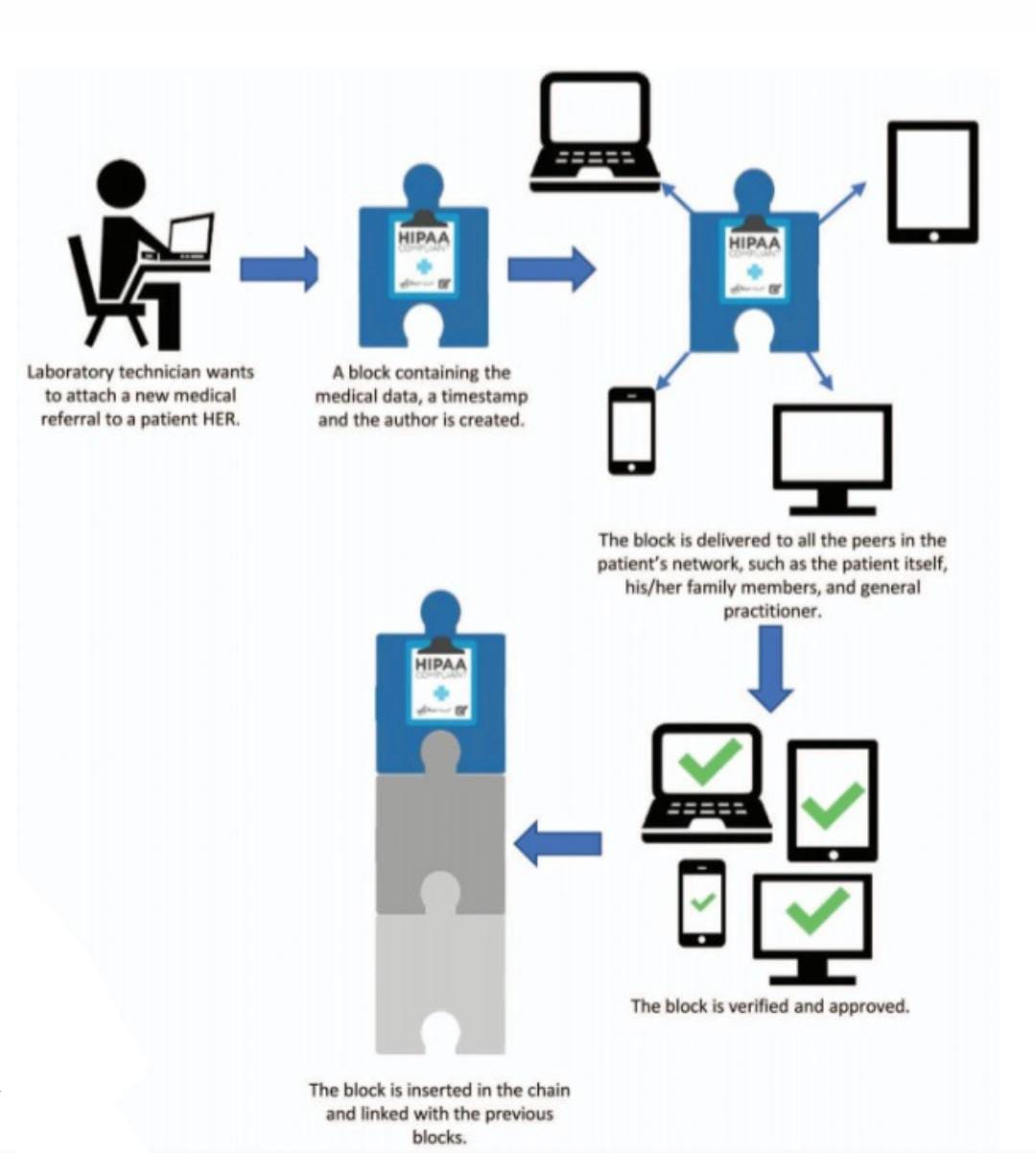
Your patients have watched the news. They have heard about hospital systems getting hacked, personal data being sold, and medical records being leaked.
When someone is dealing with epilepsy, early-onset dementia, or chronic pain conditions, they are already vulnerable.
The last thing they want to worry about is their neurological diagnosis becoming public knowledge or affecting their job prospects.
What patients are actually thinking: “If my employer finds out about my seizure disorder, will it affect my career? If my insurance company sees how often I need MRIs, will they drop me? If someone hacks this system, what happens to the most private parts of my life?”
The honest approach should be to not lead with “cutting-edge blockchain technology.” Lead with understanding: “We know that your neurological health information is deeply personal. You are trusting us with details about your brain, your symptoms, your fears, and we take that responsibility seriously.”
Instead of tech jargon, explain the actual protection to make it meaningful.
For example, “Your medical records are secured in a way that makes them virtually impossible to alter or access without your permission. Even if someone tried to hack our system, your information would remain locked and unusable to them.”
You can have a real conversation with your patients about data security, like “I know you are worried about your memory issues affecting your job. The way we protect your information means that what we discuss here stays here – period. Your employer, your insurance company, and even other doctors can only access what you specifically choose to share.”
What this actually builds is trust. Not because you are using fancy technology but because you are addressing the real fear behind the need for that technology.
Patients relax into treatment when they know their most vulnerable moments are truly protected.
Here’s what your patients are dealing with: they have a condition affecting the most complex organ in their body, and they can’t see it, touch it, or understand how it works. You are asking them to trust treatments for something that feels completely abstract.
The real struggle is when you tell someone they have a lesion on their frontal lobe; they nod politely, but inside, they are thinking, “What does that even mean? What does my brain actually look like? How big is this problem?” They go home and try to Google brain anatomy, but it’s all medical illustrations that don’t connect to their lived experience.
VR is that lightbulb moment when the abstract becomes concrete. It’s watching a patient with MS finally see their myelin sheath and understand why certain movements are difficult.
It’s helping someone with a brain tumor visualize exactly where it is and why their specific symptoms make perfect sense.

Instead of saying, “You have damage to your motor cortex,” you take them on a journey through their own brain. They see the healthy tissue, they see the affected area, and suddenly, their tremor isn’t just happening to them; they understand the why behind it.
When a patient says, “Oh my God, now I get it,” it is the moment that matters. “That’s why I have been having trouble with words; it is right there.” Fear of the unknown transforms into understanding something specific and manageable.
To make it personal, use VR to show their actual scans, their specific condition, and their individual treatment approach. “This is your brain, this is your lesion, and here’s exactly how the medication we are prescribing will help this specific area.”
The real value isn’t in technology. It’s in the conversation that happens afterward. Patients ask better questions, follow treatment plans more consistently, and feel like active participants instead of passive recipients of care.
Instead of patients leaving your office confused and Googling their condition, they leave with clear mental images of what’s happening and why your treatment approach makes sense.
They become partners in their care because they finally understand what they are partnering with.
Also See: Healthcare Digital Marketing: Best Practices To Follow
The convergence of rapid market growth, changing patient behaviors, and technological capabilities creates a defining moment for neurology practices. The data is clear: practices that successfully integrate these human-centered approaches to technology adoption will capture a disproportionate market share in a growing field.
The practices thriving through 2030 won’t be those with the most advanced technology but those who use technology to solve the core challenge of neurological care: helping patients understand and manage conditions affecting an organ they cannot see or directly monitor.
Whether through telemedicine that meets patients in their daily reality, AI tools that provide empathetic guidance during frightening moments, or VR experiences that make the abstract tangible, the goal remains consistent: transforming fear and confusion into understanding and partnership.


